How to Talk to Children About Mental Health and Suicide

Resilience is a trait commonly used to describe children — and in many ways, it’s true. Generally, children are naturally optimistic, adaptable and can surprise adults by bouncing back after challenges and setbacks. However, while they’re resilient, children can also experience stress and traumatic events that cause mental health struggles.
Because children may not always know how to communicate their thoughts and feelings, parents and caregivers need to take time to initiate conversations about mental health. When caregivers start the conversation, they establish trust with their children. The result? Children feel confident talking about mental health too. Discover why it’s important to talk about mental health with children, how the conversation should shift with age and when to evolve the conversation to include self-harm and suicide.
To better understand your child and start a conversation about mental health, download our FREE mental health assessment now.
Why it’s Important to Talk About Mental Health
Even though it’s complex, and caregivers might not want to think that their child would ever struggle, it’s crucial to open up a conversation about mental health. Children as young as two or three years of age can begin to learn, understand and gain value from mental health check-ins.
The Current State of Mental Health in Children
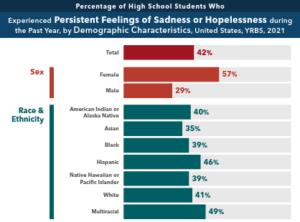 The number of children living with mental health challenges in the United States has reached an all-time high. Recent research shows an increase in children feeling persistent sadness, hopelessness and suicidal thoughts by about 40%. The pandemic isolation contributed to the increase, but why have these numbers been on the rise for years?
The number of children living with mental health challenges in the United States has reached an all-time high. Recent research shows an increase in children feeling persistent sadness, hopelessness and suicidal thoughts by about 40%. The pandemic isolation contributed to the increase, but why have these numbers been on the rise for years?
Matt Arnet, Director of Outpatient Services with KVC Kansas, has observed that the expansion of smartphones, tablets and social media has contributed to the constant stress. Using these devices creates an opportunity for bullying outside of in-person interaction and noticeable isolation from peers for being different. Social media, pressure to do well in school and family interactions are a few reasons children struggle with their mental health.
“We’ve learned over the last 20 years or so that mental and physical health are directly linked,” Arnet says. Studies have shown early adversity and trauma can disrupt a child’s brain development and compromise the proper functioning of their immune and nervous systems leading to delays and even health issues into adulthood.
Mental Health Maintenance and Communication
 Regular conversations with a caregiver are ideal for building a foundation, but children might need a mental health check-up. Like we take children to a pediatrician for physicals and regular check-ups, Arnet recommends doing something similar with mental health. It’s ideal for children eight to 18 to receive regular evaluations, like those given at KVC Kansas, for anxiety and depression or meet with a therapist for further help.
Regular conversations with a caregiver are ideal for building a foundation, but children might need a mental health check-up. Like we take children to a pediatrician for physicals and regular check-ups, Arnet recommends doing something similar with mental health. It’s ideal for children eight to 18 to receive regular evaluations, like those given at KVC Kansas, for anxiety and depression or meet with a therapist for further help.
Children may feel pressured or put on the spot with one-sided conversations focusing solely on them. Instead, you as a caregiver, can allow the conversation to go both ways. Model mental health awareness yourself by illustrating appropriate behavior. For example, if you as a parent or caregiver, are having a rough day due to stressors, talk candidly about how you’re feeling and how you’re coping.
Starting the Conversation
“Talking about mental health with children early helps them understand if something they’re feeling is part of the normal ups and downs of life or something outside the realm,” Arnet says.
In addition to checking in with children today, mental health conversations can have a ripple effect for tomorrow. Building mental health awareness can help them with coping skills and self-care as they grow, reducing the risk of suicide. Plus, children can build empathy for those around them in the future, creating a toolkit to support classmates and friends if they face a mental health challenge, perhaps even helping to prevent suicide in their community.
So how can you get started? Arnet suggests dedicated family time when it’s possible. “It can be challenging to find time,” he acknowledges. “But mealtimes, or even during car rides, can be a great place for a little check in: ‘How is everyone doing?’ Make it a platform where everyone is checking in, even adults.” This communicates to children that mental health is important — and illustrates it’s a safe environment where children can come forward with something causing them distress, he advises.
How Mental Health Conversations Change with Age
Just as a child’s understanding changes with age, the conversations must also change, grow and deepen. Working with children on mental health can begin as early as two to three years old and evolve through their childhood phases. Along with the conversations, watch for behavioral or emotional changes that may signal the need for professional treatment.
Toddler to Younger Elementary Age
 For younger children, mental health education can start with equipping them to label or describe their emotions. “It’s important, even at a young age, to help kids be aware of their emotions, behavior and temperament,” Arnet says.
For younger children, mental health education can start with equipping them to label or describe their emotions. “It’s important, even at a young age, to help kids be aware of their emotions, behavior and temperament,” Arnet says.
Conversation Focus: Start by checking in on how they’re doing. Keep it simple with happy, sad, angry and excited, and include more subtle expressions as they mature. Add basic labeling of feelings and emotions as they happen. For example, “This makes me feel angry because…” Or “I feel happy today.”
Older Elementary Age Through Middle School
During this period of growth, a child’s understanding and mental complexity change rapidly. They’re learning about social relationships, working through disappointments and rejections, and becoming more naturally independent from their family system. In turn, their ability to comprehend more advanced themes of mental health grows.
Conversation Focus: Instead of sticking to the basic feelings of anger, happiness, sadness, etc., begin to get more detailed and nuanced. Introduce some subtle emotions, like disappointment, frustration, hurt and worried. Let children discuss their world and listen for queues where they need support.
High School into Young Adulthood
 As independence increases, so does the child’s ability to test limits and learn lessons. Many of these experiences will affect the child’s mental health, and additional check-ins and conversations might be necessary. Since this age group can be reluctant to chat, picking the right time and managing fallout is necessary.
As independence increases, so does the child’s ability to test limits and learn lessons. Many of these experiences will affect the child’s mental health, and additional check-ins and conversations might be necessary. Since this age group can be reluctant to chat, picking the right time and managing fallout is necessary.
“As kids get past elementary school, their brain development is rapidly increasing and they understand more about life,” Arnet says. “They’ve had experiences with adversity, disappointment and other complicated feelings.”
Conversation Focus: Listen in a non-judgmental way. Ask clarifying questions like “Can you explain how this situation makes you feel?” Make sure to keep the conversation confidential to maintain trustworthiness. You can also model smart mental healthcare yourself, and let children into your own world when it’s safe and appropriate.
Evolving the Everyday Mental Health Conversation into Discussing Suicide
If you or someone you know is considering suicide, call or text the Suicide and Crisis Lifeline at 988 or chat live at 988Lifeline.org. If you’re in Kansas or Missouri, you can also call Camber Mental Health at (913) 890-7468 to find children’s mental health treatment near you.

At some point, the conversation may need to discuss suicide risk and self-harm. Every year, approximately 45,000 Americans die by suicide. In 2020, suicide was the second-highest cause of death in Americans ages 10 to 14.
“As we talk with older kids about mental health, we have to be open about it — that sometimes those feelings become so big, it’s hard and we sometimes don’t know if we can handle it anymore,” Arnet says.
For younger children, Arnet explains that children as young as six years old are familiar with the idea of self-harm and suicide. Young children are often experiencing some big emotions for the first time, and those emotions can feel too big to handle — and they may not fully grasp the full trajectory of self-harm.
“These are some of the toughest conversations,” Arnet acknowledges. “But we know from working with children at KVC, especially at KVC subsidiary, Camber Mental Health, that kids as young as six or seven years old use self-harm language.”
Children may not understand that if they hurt themselves, it can have serious long-term implications. While having these conversations, parents and caregivers can be direct with children on self-harm and suicide. Let children know that when they’re struggling with big feelings and have thoughts of suicide, they need to reach out to a person they trust and get help.
For older children, open communication is crucial. They’ve likely heard about suicide and self-harm from school and the media, so caregivers have a golden opportunity to foster an environment of open communication. Practice non-judgmental conversations so your teen feels safe to be vulnerable. Be prepared to listen and empathize, even if you don’t understand.
Validate these feelings if your teen mentions they’re struggling (or that someone they care about has expressed that). “Make sure your teen knows that when they have feelings like this, it’s okay, and it’s time to talk to someone they trust,” says Arnet. “These conversations can really pay off later if and when a child is in crisis, and they’ll know that they can get the help they need and it won’t be punitive in any way.”
Finding Help and Hope with KVC Kansas
Here at KVC, we know we all need connection. When you’re looking for therapeutic services for your child, things can feel hopeless. But we’re here to help. KVC’s licensed therapists provide quality mental healthcare by developing trust and treating the whole person. Our mental health professionals offer individual and family therapies to children and families involved in the child welfare system. We work to meet the needs of children, adolescents, and adults so they can meet their full potential at home, school, and work. Learn more about our outpatient therapy services.
